The Full Spectrum of GLP-Agonist Medication: A Diabetes Patient's Comprehensive Guide
Living with diabetes means someone must constantly navigate decisions about the foods they eat, the physical activity they undertake and the medication they rely upon. Today, the landscape of diabetes care is evolving rapidly, with a keen focus on cutting-edge treatments that can effectively manage blood sugar while reducing the risk of complications. One such revolution is the advent of GLP-Agonist medications, a class of drugs heralded for their efficacy in diabetes management. Here, we'll unpack everything diabetes patients need to know about GLP-agonists — from how they work to what to expect from using them.
Unveiling the Mechanism of GLP-1 Agonists
But what are GLP-agonists exactly? They form an essential part of modern diabetes medication. GLP stands for 'Glucagon-Like Peptide'. The drugs in this class of medicine act similar to the GLP-1 hormone which our bodies make on their own. These hormones are triggered when we consume food and they affect our feelings of satiation. The key characteristic of GLP-1 agonists is their ability to stimulate insulin secretion while suppressing glucagon — a hormone that raises blood sugar levels. Because a GLP-1 agonist affects the GLP-1 hormone they contribute to our stomach’s rate of emptying which consequently provides a feeling of fullness. That in turn helps people helps control their appetite. Known for their multi-pronged approach to glycemic control, GLP-1 agonists have redefined the standards of diabetes care.
The Leading Brands of GLP-Agonists
Numerous brands of GLP-agonists are available in the market today, each with its unique set of attributes. Some of the commonly recognized names include:
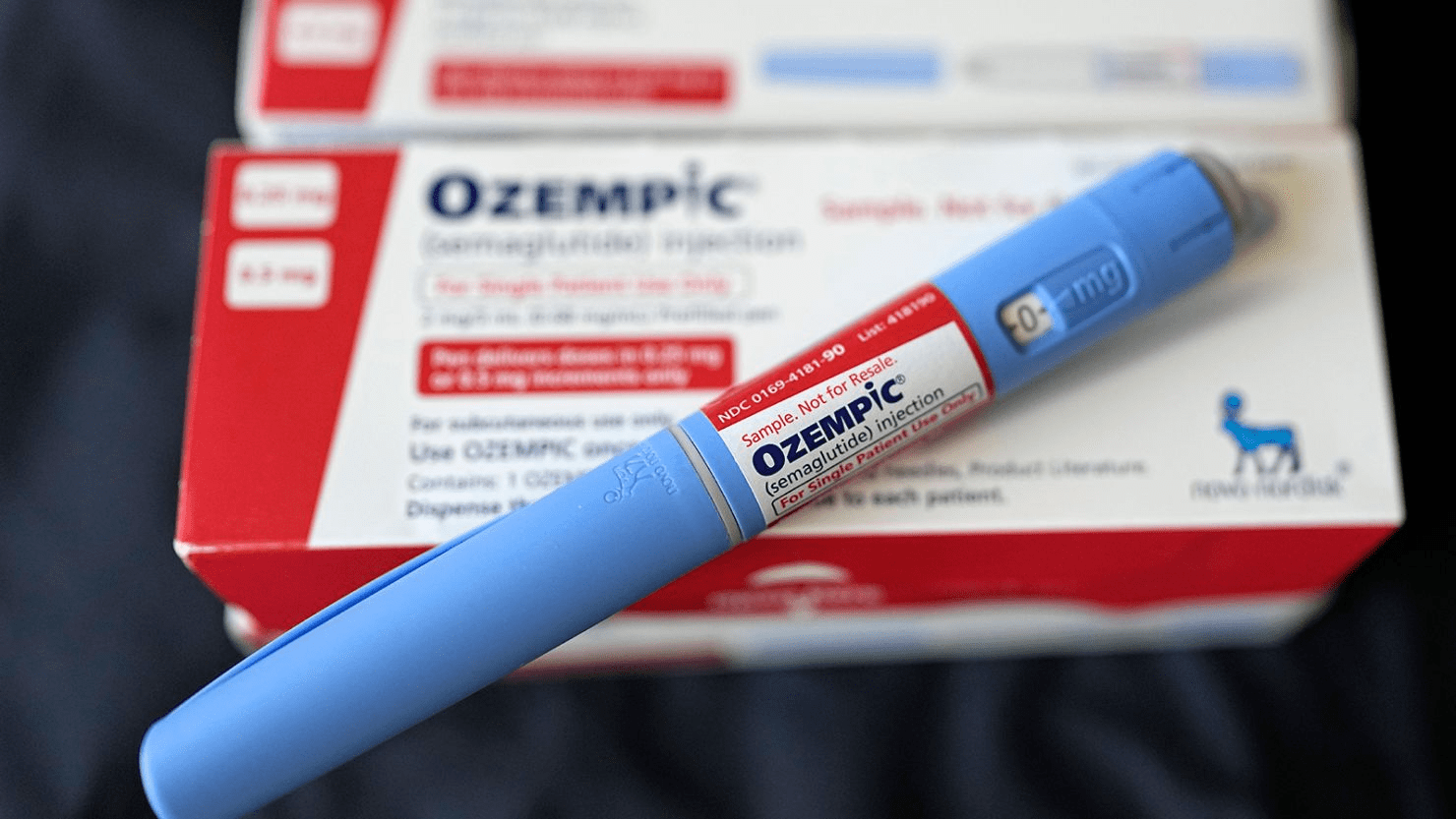
- Ozempic (semaglutide): A well-established therapy with a once-weekly dosing schedule.
- Bydureon (exenatide extended-release): A pioneer in the field with a once-weekly pen for convenient dosing.
- Rybelsus (oral semaglutide): For those averse to injections, this is the first and only oral GLP-1 agonist available.
- Victoza (liraglutide): Another seminal product offering daily dosing for heightened flexibility.
- Trulicity (dulaglutide): Known for its straightforward, once-weekly injection regimen, increasing patient adherence.
- Wegovy (semaglutide): New on the scene, approved for chronic weight management in obese or overweight adults with type 2 diabetes.
The Science Behind GLP-1 Agonists and Diabetes Management
GLP-1 agonists are engineered to work in harmony with the body's natural processes, yet they offer a therapeutic edge that can significantly impact the health of those managing diabetes. Their key benefits include:
Enhanced Glycemic Control
By promoting insulin secretion and inhibiting glucagon release, these drugs help regulate glucose levels after meals, often reducing the need for additional short-acting insulin.
Weight Management
GLP-1 agonists are known to benefit individuals by supporting efforts to maintain or lose weight, a critical aspect of diabetes care given the link between diabetes and obesity.
Cardiovascular Health
Certain GLP-1 agonists have been proven to reduce the risk of cardiovascular events in patients, marking a milestone in diabetes treatment.
Potential for Renal Protection
Emerging studies suggest GLP-1 agonists may offer protective effects for the kidneys, an organ system often affected by diabetes complications.
Combining GLP-1 Agonists with Other Diabetes Medications
The comprehensive approach of GLP-1 agonists makes them an excellent candidate for combination therapy. They can be used alongside other oral antidiabetic drugs, insulin, and even SGLT-2 inhibitors, offering a range of options to create personalized treatment regimens that best suit patient needs.
Synergies with Sulfonylureas and DPP-4 Inhibitors
When paired with these medications, GLP-1 agonists can lead to a greater reduction in blood sugar levels and often require lower doses of concomitant drugs, potentially minimizing side effects.
Complementing Insulin Regimens
For those requiring insulin, adding a GLP-1 agonist can potentially reduce the required insulin dose, aiding in weight management and lowering the risk of hypoglycemia.
The SGLT-2 Inhibitor Connection
Studies are underway to explore the synergistic benefits of GLP-1 agonists and SGLT-2 inhibitors, which can result in improved heart and kidney health.
Understanding the Side Effects of GLP-1 Agonists
Like all medications, GLP-1 agonists do come with potential side effects. GLP-1 Agonists are relatively new so there is still much to learn about side effects, but some of the better known side effects are related to gastrointestinal issues. For example prolonged nausea and vomiting, which can sometimes last weeks or more, gastroparesis or stomach paralysis. Some side effects such as diarrhea or constipation are often transient and can diminish as the body gets used to the GLP=1 medication. Rarely, more severe side effects like pancreatitis or medullary thyroid cancer may occur but are not common.
As with any new medication, it’s important that patients discuss the risks vs. rewards of a GLP-1 agonist with their healthcare provider.
The Prevalence of GLP-1 Agonists in Diabetes Care
The popularity of GLP-1 agonists has surged in recent years, driven by their efficacy and patient-friendly dosing schedules. They have become a preferred choice for doctors seeking to optimize diabetes management, particularly when weight loss or cardiovascular protection is a primary goal.
Success Stories and Patient Satisfaction
Many individuals who have incorporated GLP-1 agonists into their diabetes treatment plan report significant improvements in their quality of life, often including better blood sugar control, weight loss, and reduced insulin needs.
Physician Endorsement and Guidelines
Most diabetes treatment guidelines now include GLP-1 agonists as part of the standard therapeutic armamentarium, reflecting the strong endorsement from the medical community.
Pharmaceutical Innovation and Future Prospects
Pharmaceutical companies continue to invest in developing new formulations and expanding indications for GLP-1 agonists, signaling a strong commitment to innovation and improvement in diabetes care.
When the Best Isn’t Available: GLP-1 Agonist Shortages
Despite their growing prevalence, patient experiences with GLP-1 agonists have been marred by intermittent shortages. These supply disruptions can be a source of significant stress for individuals who depend on these drugs for their daily management.
The Real Impact on Diabetic Patients
For those with diabetes, adjusting to sudden changes in medication can be unsettling and may affect their health outcomes. It's important for patients, and their healthcare providers, to stay abreast of medication access challenges and make sure they have a plan to navigate the instances when this problem may arise.
Mitigation Strategies During Shortages
When faced with a shortage, it’s important to work closely with healthcare providers to explore alternative medications or treatment approaches. Additionally, staying in touch with patient advocacy groups can provide support and access to the latest information.
The Future of Diabetes: The Promise of GLP-1 Agonists
The journey with diabetes is ever-evolving, and the role of GLP-1 agonists in this narrative continues to unfold. With their multifaceted benefits and growing body of evidence supporting their use, it's clear that these medications are set to play a pivotal role in the fight against diabetes.
Embracing the potential of GLP-1 agonists means not just understanding the science but also being prepared for the challenges and embracing the exciting opportunities they bring to diabetes management. As we look forward, the message to patients is clear: in the world of diabetes care, new allies are constantly emerging, ready to join the battle alongside you and your healthcare team.
